Marjorie is an 85 year old lady who is taken ill at home. An ambulance is sent following a 999 call. The Ambulance Service book her onto their system and record that she is being brought into her local hospital. At the hospital the Emergency Department and the control room know she is coming as she appears on the ambulance arrivals boards located in the both locations. Marjorie arrives at the department and is booked in by the admin team. She is already known to the trust and easily identified on the System and a new attendance recorded. The ED Clerk notices there is a safeguarding alert and communicates this fact to the admitting nurse who is performing triage. Marjorie appears on the ED System and the electronic whiteboards located throughout the department.
 ED Whiteboard
ED Whiteboard
Her status and location (currently in the ambulance handover area) are tracked as she progresses on her journey. Staff can see the forget-me-not symbol on the boards, indicating that Marjorie is known to have a pre-existing diagnosis of Dementia, this being recorded on a previous attendance. This board shows Frailty flags, Ceiling of Care, GAPS and NEWS.
A few minutes later the performance activity dashboards are updated.
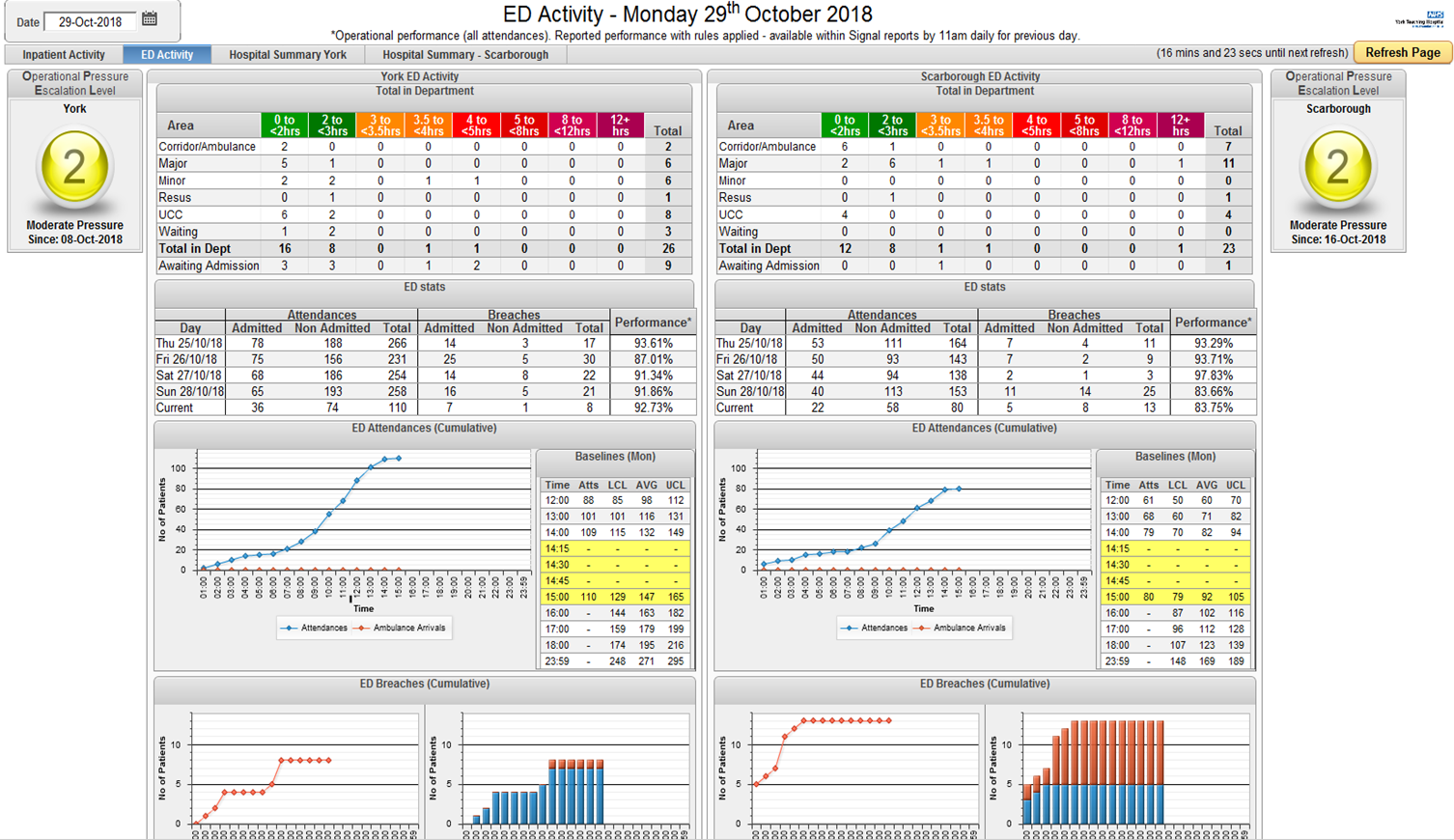 Near real-time dashboard
Near real-time dashboard
Following the handover to the ED team The Nurse completes a set of physiological observations, recording vital signs on CPD. This automatically calculates a e-NEW score of 5 and triggers a prompt for a sepsis screen. A NEW score of 5 is the recommended trigger point for sepsis screening and the system automatically delivers an alert with prompts for action.
A sepsis screen task appears on the ED board against her listing.
The nurse takes bloods to complete a sepsis screen as result of that alert. The sepsis order blood set is pre-filled automatically when launched from within the sepsis screen. This reduces the time taken in ordering.
Marjorie is moved to a different bay and the system updated. Her location is updated throughout the system and all the electronic whiteboards in the department are updated automatically, clearly showing the NEWS of 5, the Dementia alert and other key information.
The admin team access the enhanced summary care record on the national system and upload onto the system. From this point on access to the summary care record is then instant and directly in context within the clinical system.
The system, including the electronic ED whiteboard has a symbol highlighting to the clinical team that during this patient’s last stay it was recorded that she had a DNACPR form completed. This indicates that the patient was for “active ward level care” but not for escalation to intensive care. The registrar, phones the next of kin, Marjories daughter, to confirm this fact (the phone number is on patient’s ribbon on the patient record). With permission granted, Julie completes a replacement form as the original is still at home in the kitchen. The doctor takes the opportunity to discuss the diagnosis and treatment with Marjories daughter.
Julie examines the patient and makes an early assessment that the patient will most likely need to be admitted and records this on the electronic record. She goes to order bloods electronically but is warned that they have already been requested. She orders a Chest Xray, updates the ED record and records an outcome of “requiring admission to AMU” with a diagnosis of sepsis. The NEW score of 5 prompts the requirement for a discussion with the admitting specialty so that the team are aware that this patient is unwell and high risk. Recording the patient as an intended admission causes Marjorie to become visible on the Admission Board, on the ward-list of the Admissions Unit (AMU) as a pending admission and on the bed managers boards in the control centre and bed managers office. The ward staff can see the alert flag indicating that Marjorie is recorded as MRSA positive from previous admissions and they plan allocating her to a side-room.
 Arrivals Board
Arrivals Board
Back in ED the inpatient clerking in process is started and all Marjorie’s medications are written up on EPMA including her ongoing antibiotics. Many of her medications are suspended given her critical illness but recorded as such so that they are not forgotten come time for her discharge.
Her ECG is completed in ED and the printout is scanned onto the system along with the “CAS Card” these becoming visible within the electronic record to the team on AMU. Marjorie is moved to AMU and her ED attendance is completed within the ED screens. The electronic summary is transmitted electronically to her GP.
On arrival on AMU her “pending admission” is finalised with a few clicks and Marjorie is allocated a bed. All the whiteboards and systems update. The inpatient record is explicitly linked to the ED record with data such as reason for admission flowing through to the inpatient care record.
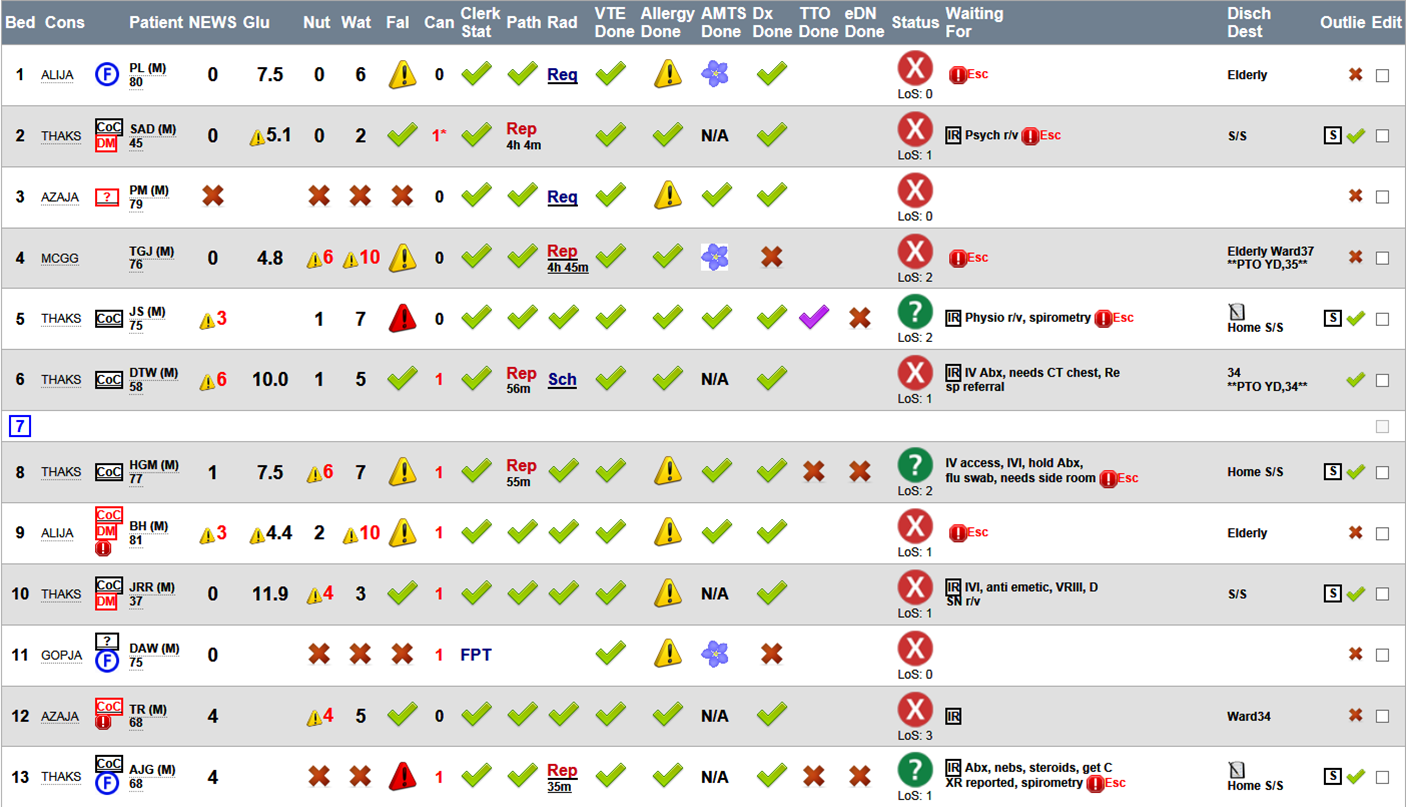 Patient Safety Board
Patient Safety Board
The arrivals board on AMU shows that Marjorie needs her nursing assessments completing for pressure area and falls risk. Her status as a diabetic is clearly visible on the whiteboard (having had a referral for diabetes retinal screening 10 years prior she has been identifiable as diabetic since then). Four times a day blood glucose monitoring is automatically scheduled as part of her observation regime. The diabetes register also makes her clearly visible to the diabetes specialist nurses in the hospital. Her glucose on admission is 17 so she also appears on their ‘out of range list’.
The admitting team clerk her in and notice her blood results are back as highlighted on the ward-list and patient board symbols. If not as they exit the patients record they get an interruptive alert to highlight that unacknowledged results are available and are led to the appropriate screen to confirm the results. The patient has results (creatinine has risen 1.5x previous median) indicating an acute kidney injury and the doctors have access to a checklist bundle if unclear on how to proceed. This reminds them to order a renal ultrasound. The doctor also notices that the patient has a chronic condition recorded as a chronic diagnosis (CKD-5 for conservative care). This confirms that she has already advanced kidney failure but is known to the renal team and is for conservative care. They realise that dialysis has previously been considered and ruled out as a treatment option. That prompts the doctors to access the renal letters using the casenote library applying the nephrology filter to hasten access to the relevant information
The blood results also show a raised bilirubin (yellow) and the old radiology results indicate that the patient is known to have gallstones. These facts add up to biliary sepsis secondary to obstructive jaundice from gallstones as a likely unifying diagnosis. The doctor adds a gastroenterology referral from within the patients EHR so that the gastro team pick up the referral at start of play the following morning. In the morning the patient appears on the gastro teams wardlist identified as a new referral. The renal team appear to input to her care as she is on their list as well. They have previously tagged her as a conservative care patient with advanced renal failure so appears on the renal ward list whenever she is admitted to hospital so they can assist in her care given her specialty needs with prescribing in advanced renal failure.
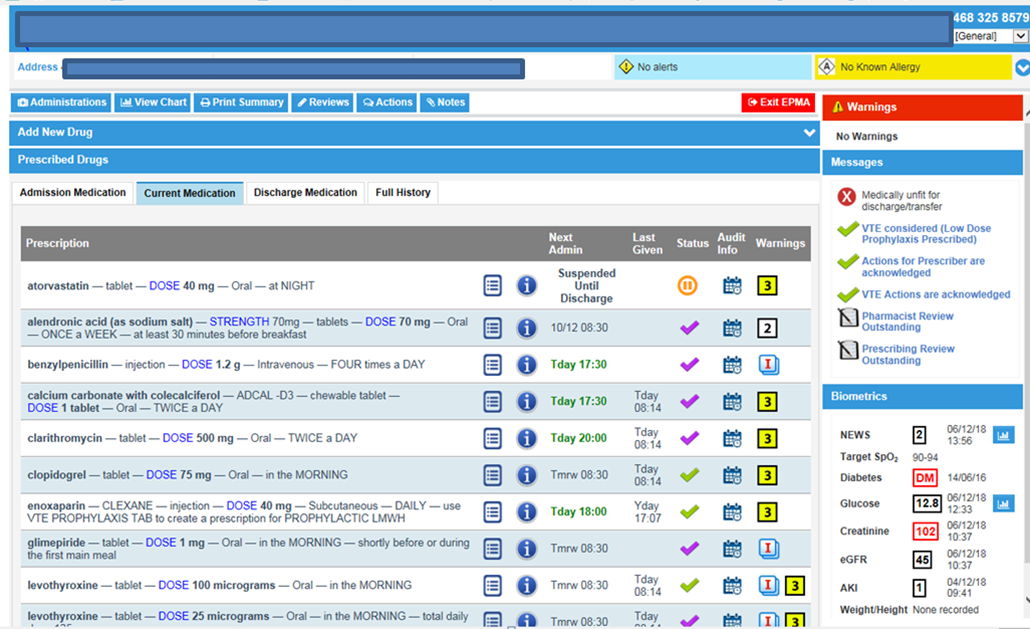
They remotely adjust the doses of her painkillers and her antibiotics. Her kidney function (eGFR) is presented within the electronic prescribing system which is a fully integrated system. As the gastro team arrive the patient is called for ultrasound as the request was on the radiology worklist when the radiology department opened at 0830 and there was a slot available first thing. She is transferred to Elderly Medicine and a transfer form generated.
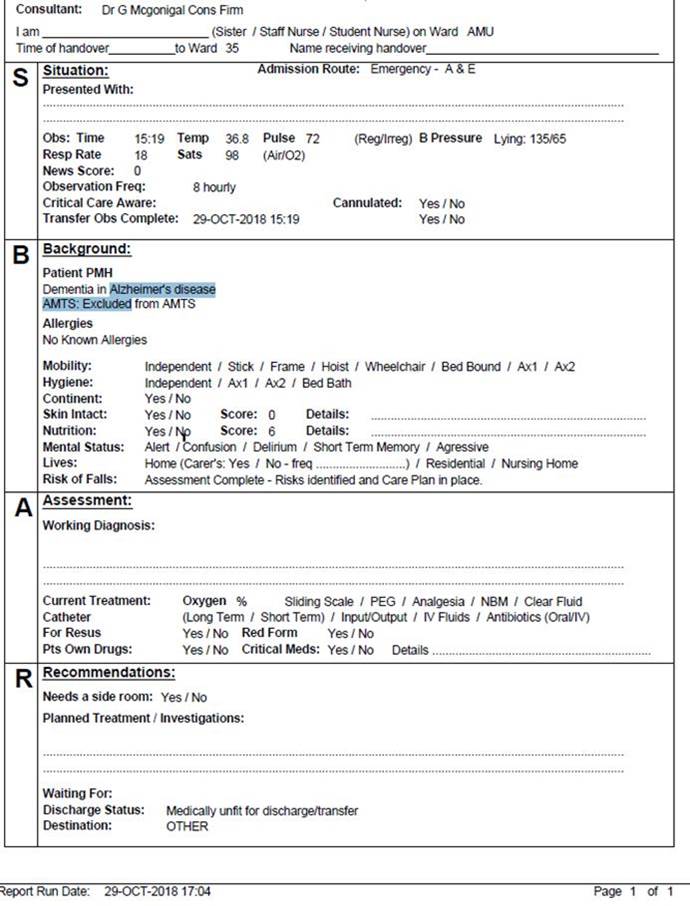
Later that morning the patient is transferred to an elderly care ward. A transfer form is created from the EHR using an SBAR format to reduce duplication of effort by staff.
Recognising the dementia label the bed managers ensure it is likely to be her last move within the hospital to minimise disruption and delirium. All her forward blood test results (standing order created for 3 days by the staff) ‘move’ with her as she changes ward. The phlebotomy team identify all the requests due each morning from their worklist linked to all patient records updating their location in real time.
The Discharge letter is finalised by the discharging doctor who selects TTO Meds which are then flagged up on the screens within Pharmacy and recorded on the Discharge Notification having been electronically validated by the ward Pharmacist. Once the TTO pack is returned to the ward Marjory is discharged by the Nurse, given a paper copy of the dischareg notification and discharged from the Inpatient screens. At this point the electonic version of the discharge notification is transmitted directly to the GP system. A Few hours later Blood results are posted in the pathology department. Because Marjory is no longer an inpatient they cannot be seen on the ward, instead they become visible on the Consultants “Notify” (their clinical workflow system) along with worklist item to do a full discharge Letter.